Modern Care Deserves Modern Reimbursement
Cardiac remote monitoring plays a vital role in proactive care, helping patients avoid complications and reduce hospital visits.1 As care standards evolve, aligning reimbursement with today’s clinical reality is essential to uphold guideline-directed remote monitoring.
Get InvolvedRevaluing CPT Code 93296
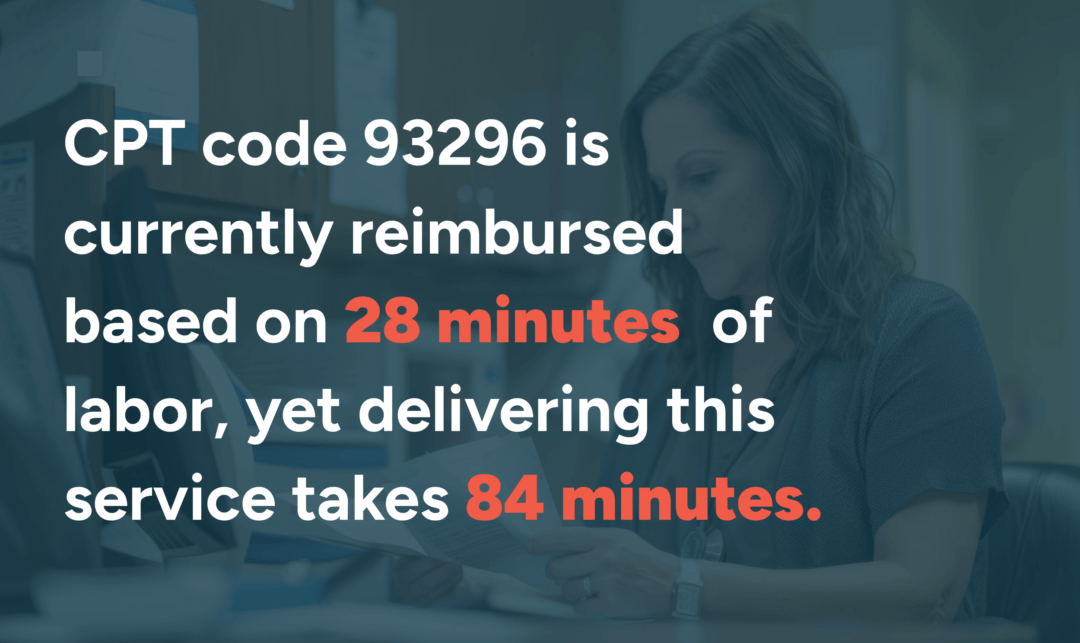
CPT code 93296 represents the technical work behind remote monitoring of patients with implantable pacemakers and defibrillators (CIEDs). The inputs used by Centers for Medicare & Medicaid Services (CMS) to calculate reimbursement in 2018 no longer reflect the realities of modern remote monitoring.2
What This Means
Guideline-directed remote monitoring as stated in the 2023 HRS Consensus Statement is economically unfeasible. Outdated reimbursement is forcing clinics to absorb unbearable financial losses, threatening equitable patient care and making remote monitoring unsustainable.
- Clinics face a $60.16 reimbursement shortfall per patient every 90 days—adding up to a $240,640 annual deficit per 1,000 patients.3
- Staffing shortfalls of 0.5 FTE per 1,000 patients lead to burnout, alert backlogs, and reduced remote monitoring capacity.3
- Delayed response to critical alerts may increase the risk of hospitalization, ER visits, and worsen outcomes.
- Patients receive less education and technical support, driving noncompliance and disengagement.
- Clinics may be forced to limit enrollment, especially for rural or underserved populations, leading to wider health disparities.
Advocating for Fair Reimbursement
Vector Remote Care helped lead the formation of the Cardiac Device Patient Monitoring Association (CDPMA) and has submitted real-world data to CMS, highlighting the gap between current reimbursement for CPT 93296 and the true cost of delivering guideline-directed care for CIED patients. Together, we are advocating for updated rates to reflect today’s clinical demands and safeguard access to high-quality remote monitoring.
- What We Propose: Raise reimbursement from $19.41 to $79.57 by updating outdated CMS inputs—labor time, staff classification, equipment costs, and RVUs.4
- Why It Matters: Aligning payment with real costs enables clinics to staff appropriately, process alerts faster, and sustain the impacts of growing patient panels.
- The Impact: Clinics can continue delivering timely, equitable care—and patients stay connected to remote monitoring, a Class 1A recommendation, without interruption.1
Stay Informed & Show Your Support
We’re collaborating with national leaders—including the Heart Rhythm Society and the American College of Cardiology—to advocate for fair, sustainable reimbursement. Your voice strengthens this effort.
Join us to help ensure remote cardiac monitoring remains accessible, effective, and supported for every patient who needs it. Sign up below to stay informed and learn how you can participate in this initiative:
Sources & Supporting Data
- HRS/EHRA/APHRS/LAHRS Expert Consensus Statement on Practical Management of the Remote Device Clinic. Heart Rhythm, 2023. Link
- CY 2018 Medicare Physician Fee Schedule Final Rule. Centers for Medicare & Medicaid Services, 2017. Link
- Calculations based on a clinic size of 1,000 patients per 90-day cycle. CMS-recognized labor (467 hours ≈ 0.3 FTE) versus actual required labor (1,394 hours ≈ 0.8 FTE) results in an unfunded staffing gap of 0.5 FTE. At a reimbursement shortfall of $60.16 per patient, this equates to an annual deficit of $240,640 per clinic.
- The $19.41 reimbursement rate is the 2025 national average. Actual reimbursement varies by Medicare Administrative Contractor (MAC) locality. To find your region’s rate, visit the CMS Physician Fee Schedule. Link